
Fourth Trimester, Mental Health
Post-Partum Depression: Moving Out of the Shadows into a Community of Support
| Post-partum depression (PPD), the most common complication of pregnancy, is finally transitioning from a topic discussed behind closed doors to being in the national headlines. The Food and Drug Administration’s announcement that it has approved the first drug (brexanolone) to treat post-partum depression dominated the news cycle recently. Meanwhile, celebrities are using their national media platforms to share their experiences with post-partum depression. Many, including Alyssa Milano, Serena Williams, and Chrissy Teigen, have candidly admitted that their wide circle of support and access to the best medical care didn’t shield them from this condition that is experienced by as many as 400,000 American women each year.
Despite these more open discussions about PPD, we have a long way to go before women become more comfortable and confident about sharing their experiences and seeking help. Concerns or even fear about the judgment or criticism they will experience if they talk about feeling sad, inadequate, and hopeless lead to women downplaying or even hiding their symptoms. Add to that the public and personal pressures to move seamlessly and happily into motherhood, and it’s not surprising that women delay or never receive the support and help they need to manage post-partum conditions. Preparation and Understanding are Key to Knowing “It’s Not Just All in Your Head”Given the prevalence of PPD and advantages of early diagnosis and treatment, understanding what PPD is, how to treat it, and where to get help are key. There is no single cause of post-partum difficulties. Physical and emotional issues both play a role. Drops in hormone levels, including those produced by the thyroid, contribute to fatigue and feelings of sadness. Sleep deprivation and being overwhelmed with new responsibilities, as well as an inability to carve out time for self-care can worsen what new mothers are feeling physically and mentally. Post-partum medical conditions can be bucketed into three diagnoses that have different symptoms and variations in duration and treatment options:
Post-Partum Medical Conditions, Symptoms, Duration, and Treatment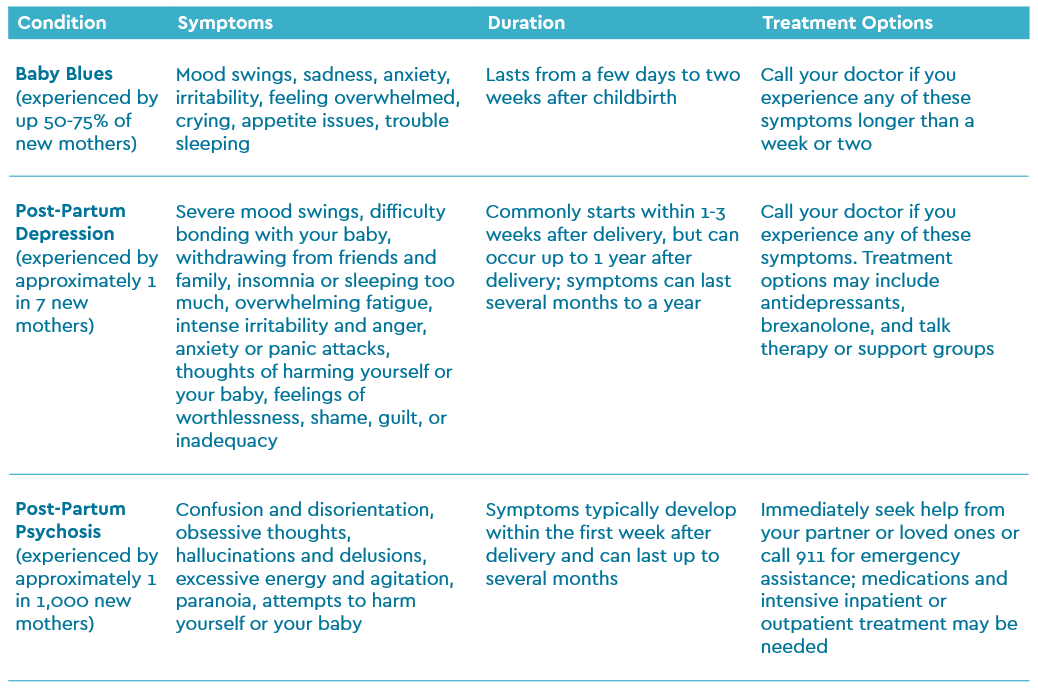
Source: Mayo Clinic. Celebrities Open Up about PPD
Post-Partum Support Options
Don’t Forget Self-CareIn addition to the treatment options noted above, ensuring that you have time to care for yourself in the weeks following delivery is not a selfish endeavor. It’s the wise “make sure your oxygen mask is secure before assisting others” mindset. Here are some ideas to consider.
How you feel after giving birth may seem like it’s out of your control, but what is within your control is getting the help and guidance you need to care for yourself and your baby. New mothers need to trust that how they are feeling is not some weakness on their part, but instead a common condition that can be treated with help from medical professionals or other support systems. And there are consequences to toughing it out on your own. Left untreated, PPD can last for months and potentially become a chronic depressive disorder. Remember, we’re here for you. This is the time in your life when being honest and open with care providers is more important than ever. Trust us with your concerns, and know that we provide a safe space for discussing post-partum conditions. |
Similar Articles

December 16, 2022

December 15, 2022

May 20, 2022











